Connect With Us
Blog

Everything You Need to Know About Corns
Corns are hard and thick areas of skin that form as a result of constant rubbing, friction, or pressure on the skin. They are patches of dead skin with a small plug toward the center. They may appear on the tops and sides of toes and can make walking painful.
Soft corns are typically thinner with a white color and rubbery texture. Soft corns tend to appear between the toes. Seed corns are another type of corn that appear in clusters and can be tender if they are on a weight-bearing part of the foot. Seed corns usually appear on the bottom of the foot and are likely caused by a blockage in sweat ducts.
While corns and calluses are somewhat similar, calluses are a bit different. Calluses are a patch of dead skin that can occur anywhere on the body. In comparison to corns, calluses are usually a bit larger in size. However, both corns and calluses are caused by increased friction on the skin.
There are some risk factors that may increase your chances of developing corns and calluses. If you have bunions, hammertoe, or a bone spur, you are more likely to develop a corn or callus on your foot.
While Corns and Calluses tend to disappear when the friction to the affected area ceases, the help of a podiatrist may be useful in the removal process. It is important to remove the dead skin around the area and this may be done in a few different ways. Moisturizing creams may be helpful in softening and removing the dead skin around the callus. You should never use razors or other pedicure equipment to remove your corns. Doing this may worsen your corn or callus and cause infection.
In some cases, corns and calluses may be caused by abnormal foot structure or walking motion. In such a case, you should seek a podiatrist’s assistance in order to correct the issue.
Solutions for Cracked Heels
Cracked heels can make life very frustrating and embarrassing when displaying the bare feet. Aside from being unpleasing to the eye, they can also tear stockings and socks and wear out shoes at a faster rate. When severe, cracked heels may cause pain or infection.
Cracked heels are a problem for those who are athletic, those who may walk a lot, and those who have especially dry skin. Those who use medication that dry the skin, those who swim often, wearing certain types of shoes, and those who are diabetic may have trouble with cracked heels. Seniors whose skin produces less oil may also have trouble with cracked feet. There is no one way to develop cracked feet, and there is no cure.
Today, the market consists of numerous products that have a variety of ingredients to promote healing. Some of these are over-the-counter. Others are prescribed by a doctor, especially for those who have chronic dry feet and heels.
Some doctors recommend wearing socks at night for those with rough skin. This helps further healing, and helps creams stay on longer and better absorb into the skin.
One way to alleviate dryness that causes cracked heels is by using moisturizers both day and night. Another way is to make sure the skin is clean and dry at all times. Using a pumice stone to buff away dead skin before putting on moisturizer can also help. Cracked heels will not respond to the cream unless the outer layer of skin is first removed through exfoliation. After exfoliation, lotion or ointment will be absorbed by the skin more easily.
Foods that produce healing and balance can also help the skin from within. Everything that is put into the body can either help it or hurt it. Taking supplements of omega-3 fatty acids and zinc can also be very beneficial.
Nevertheless, not all products are guaranteed to help treat cracked feet. Seeing a professional is best if other treatments options were unsuccessful. A podiatrist should be able to give the best advice to help with this problem.
When Should I See a Foot and Ankle Surgeon?
 Most injuries and diseases of the foot and ankle are not treated surgically. However, a foot and ankle surgeon can still help you by examining your feet and ankles when you experience pain or other symptoms of injury or disease. You may want to consult a foot and ankle surgeon if you have sustained an injury, such as a sprain or fracture, have a medical condition that can affect the feet, have difficulty completing daily activities, or notice a change in the appearance of your feet or ankles. Foot and ankle surgeons tend to only suggest surgery when a problem is severe and non-surgical treatments have failed. For more information about how a foot and ankle surgeon may be able to help you, please consult with a podiatrist.
Most injuries and diseases of the foot and ankle are not treated surgically. However, a foot and ankle surgeon can still help you by examining your feet and ankles when you experience pain or other symptoms of injury or disease. You may want to consult a foot and ankle surgeon if you have sustained an injury, such as a sprain or fracture, have a medical condition that can affect the feet, have difficulty completing daily activities, or notice a change in the appearance of your feet or ankles. Foot and ankle surgeons tend to only suggest surgery when a problem is severe and non-surgical treatments have failed. For more information about how a foot and ankle surgeon may be able to help you, please consult with a podiatrist.
Foot surgery is sometimes necessary to treat a foot ailment. To learn more, contact one of our podiatrists of Sutera and Jones Surgical Podiatry. Our doctors will assist you with all of your foot and ankle needs.
When Is Surgery Necessary?
Foot and ankle surgery is generally reserved for cases in which less invasive, conservative procedures have failed to alleviate the problem. Some of the cases in which surgery may be necessary include:
- Removing foot deformities like bunions and bone spurs
- Severe arthritis that has caused bone issues
- Cosmetic reconstruction
What Types of Surgery Are There?
The type of surgery you receive will depend on the nature of the problem you have. Some of the possible surgeries include:
- Bunionectomy for painful bunions
- Surgical fusion for realignment of bones
- Neuropathy decompression surgery to treat nerve damage
Benefits of Surgery
Although surgery is usually a last resort, it can provide more complete pain relief compared to non-surgical methods and may allow you to finally resume full activity.
Surgical techniques have also become increasingly sophisticated. Techniques like endoscopic surgery allow for smaller incisions and faster recovery times.
If you have any questions please feel free to contact one of our offices located in Media, Glen Mills, Riddle Memorial Hospital, and Concordville, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Foot and Ankle Surgery
When conservative, noninvasive methods prove ineffective, surgery may be selected as the next course of action for the treatment of your foot or ankle condition. A wide number of foot and ankle surgical procedures exist, and it is up to your podiatrist to determine which intervention will be most appropriate and helpful for your case. Some surgical procedures include bunion surgery, fusion, hammertoe surgery, heel spur surgery, metatarsal surgery, nail surgery, neuroma surgery, reconstructive surgery, skin surgery, and tendon surgery. Typically, surgery is turned to as a definitive way to alleviate excessive pain or discomfort and to return your foot to full mobility.
Regardless of the location on the body, all surgical procedures require preoperative testing and examination to ensure the surgery’s success and preferred outcome. A review of your medical history and medical conditions will take place, as will an evaluation of any current diseases, illnesses, allergies, and medications. Tests such as blood studies, urinalyses, EKG, X-rays, and blood flow studies may be ordered. Because the procedure involves the foot and/or ankle, the structures of your feet while walking may also be observed by your podiatrist.
Care post-surgery will depend on the type of surgical procedure performed. Typically, all postoperative care involves rest, ice, compression, and elevation. To improve and ensure a safe recovery, your foot and ankle surgeon may also employ the use of bandages, splints, surgical shoes, casts, crutches, or canes. He will also determine if and when you can bear weight. A timely and thorough recovery is a priority for both you and your podiatrist, and carefully following postoperative instructions can help achieve this.
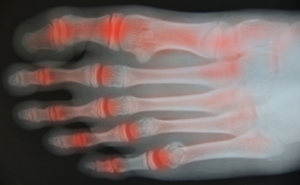
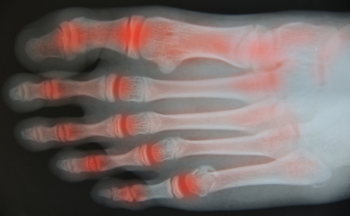
Symptoms of Psoriatic Arthritis in the Feet
Psoriatic arthritis (PsA) is a chronic autoimmune disease that affects the joints, including those on the feet. It typically affects people who have a skin condition called psoriasis. When PsA affects the feet, it produces symptoms such as painful toe swelling, joint stiffness, pain in the heels and soles of your feet, and dented or crumbling toenails. The condition has a pattern of flaring up and then subsiding. Your podiatrist can be an important part of your healthcare team when it comes to dealing with PsA in the feet. A podiatrist can help you find comfortable shoes and orthotics, maintain your mobility, and relieve symptoms during a flare up. To learn more, speak to a podiatrist today.
Arthritis can be a difficult condition to live with. If you are seeking treatment, contact one of our podiatrists from Sutera and Jones Surgical Podiatry. Our doctors can provide the care you need to keep you pain-free and on your feet.
Arthritic Foot Care
Arthritis is a term that is commonly used to describe joint pain. The condition itself can occur to anyone of any age, race, or gender, and there are over 100 types of it. Nevertheless, arthritis is more commonly found in women compared to men, and it is also more prevalent in those who are overweight. The causes of arthritis vary depending on which type of arthritis you have. Osteoarthritis for example, is often caused by injury, while rheumatoid arthritis is caused by a misdirected immune system.
Symptoms
- Swelling
- Pain
- Stiffness
- Decreased Range of Motion
Arthritic symptoms range in severity, and they may come and go. Some symptoms stay the same for several years but could potentially get worse with time. Severe cases of arthritis can prevent its sufferers from performing daily activities and make walking difficult.
Risk Factors
- Occupation – Occupations requiring repetitive knee movements have been linked to osteoarthritis
- Obesity – Excess weight can contribute to osteoarthritis development
- Infection – Microbial agents can infect the joints and trigger arthritis
- Joint Injuries – Damage to joints may lead to osteoarthritis
- Age – Risk increases with age
- Gender –Most types are more common in women
- Genetics – Arthritis can be hereditary
If you suspect your arthritis is affecting your feet, it is crucial that you see a podiatrist immediately. Your doctor will be able to address your specific case and help you decide which treatment method is best for you.
If you have any questions, please feel free to contact one of our offices located in Media, Glen Mills, Riddle Memorial Hospital, and Concordville, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
How to Care for Your Arthritic Foot
Arthritis is an inflammation of the joints and it can occur at any joint in the body, especially in the foot. It generally effects those who are older, however, it can occur at any age. Although there are many different forms of arthritis, there are three main types that occur in the foot. The three types are osteoarthritis, rheumatoid arthritis, and gout.
The primary cause of osteoarthritis is aging. As you age, cartilage degenerates around the joints which causes friction and pain. Obesity can cause osteoarthritis through mechanical stress. Injuries that damage joints can increase the probability as well. Finally, a family history of osteoarthritis can also increase chances of having it.
Rheumatoid arthritis occurs when the immune system attacks the joint linings and weakens them over a long time. While there is no known cause of rheumatoid arthritis, obesity and smoking can increase your chances of getting it. Women are also more likely to get it than men.
Gout is a form of arthritis that occurs when there is too much uric acid in your blood and painful crystals form in your joints. Men are more likely to have gout than women. People who are obese or drink alcohol often are also more likely to develop gout. Furthermore, having diabetes, heart disease, high blood pressure, high cholesterol, gastric bypass surgery or a family history of gout may increase your likelihood of developing the condition.
Symptoms of arthritis include pain, stiffness, swelling in the joints. These symptoms can make it harder and more painful to walk. Physical activity can increase pain and discomfort. Furthermore, joint pain can worsen throughout the day for osteoarthritis. Gout attacks generally last several days with the first few being the worst.
Diagnosis of gout includes either a joint fluid test or a blood test. X-ray imaging can detect osteoarthritis but not gout. On the other hand, there is no blood test for osteoarthritis. Rheumatoid arthritis is difficult to diagnosis. Doctors utilize family and personal medical history, a physical examination, and antibody blood tests to determine if you have rheumatoid arthritis.
Treatment varies for the different kinds of arthritis. Anti-inflammatory medication or steroids can help reduce pain from inflammation of the joints. Changing shoe types can help with some symptoms. Wider shoes can help with discomfort from gout and osteoarthritis. High heels should be avoided. Shoes with proper arch support and that take pressure off the ball of the foot can help with rheumatoid arthritis. Drinking lots of water can also help rid uric acid from the blood. Losing weight, improving your diet, and limiting alcohol and smoking can also help prevent or lessen the symptoms of arthritis.
If you are having trouble walking or pain in your feet, see a podiatrist to check if you have arthritis.
Plantar Fasciitis
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is the thick band of tissue that connects the heel bone to the toes. When this band of connective tissue becomes inflamed, plantar fasciitis occurs. Fortunately, this condition is treatable.
There are several factors that may put you at a greater risk for developing plantar fasciitis. One of the biggest factors is age; plantar fasciitis is common in those between the ages of 40 to 60. People who have jobs that require them to be on their feet are also likely to develop plantar fasciitis. This includes factory workers, teachers, and others who spend a large portion of their day walking around on hard surfaces. Another risk factor is obesity because excess weight can result in extra stress being placed on the plantar fascia.
People with plantar fasciitis often experience a stabbing pain in the heel area. This pain is usually at its worst in the morning, but can also be triggered by periods of standing or sitting. Plantar fasciitis may make it hard to run and walk. It may also make the foot feel stiff and sensitive, which consequently makes walking barefoot difficult.
Treatment for plantar fasciitis depends on the severity of the specific case of the condition. Ice massage applications may be used to reduce pain and inflammation. Physical therapy is often used to treat plantar fasciitis, and this may include stretching exercises. Another treatment option is anti-inflammatory medication, such as ibuprofen.
If you suspect that you have plantar fasciitis, meet with your podiatrist immediately. If left untreated, symptoms may lead to tearing and overstretching of the plantar fascia. The solution is early detection and treatment. Be sure to speak with your podiatrist if you are experiencing heel pain.
Shockwave Therapy May Help Plantar Fasciitis

The plantar fascia is located on the bottom of the foot, and connects the heel to the toes. Inflammation of the plantar fascia can cause a condition that is known as plantar fasciitis which may happen from repeated stress as a result of participating in running and jumping activities. It can affect the heel, and it is often difficult to walk. There is a treatment method that is referred to as shockwave therapy, and it may be useful in healing plantar fasciitis. It is performed by administering shockwaves to the affected area, which is typically painless. Patients are generally required to undergo three to five treatments, and relief may be found soon after it begins. Research has indicated results may be seen more quickly when it is diagnosed in the beginning stages. If you suffer from plantar fasciitis, it is suggested that you consult with a podiatrist who can determine if this is an effective form of treatment for you.
Shockwave therapy is a treatment commonly used to treat various injuries and conditions, particularly plantar fasciitis in the feet. To learn more, consult with one of our podiatrists from Sutera and Jones Surgical Podiatry. Our doctors can provide the care you need to keep you pain-free and on your feet.
Shockwave Therapy
Shockwave therapy is a new treatment option designed to treat bone conditions such as tennis elbow, shoulder pain, and others. Shockwave therapy uses high intensity sound waves that are directed to the affected tissues of the body with pinpoint accuracy. The effects are very beneficial, leading to a production of collagen fibers, eliminating inflammation.
Who Benefits from Shockwave?
Shockwave is recommended for patients suffering from heel pain and associated problems. Heel pain is a common condition which can be caused by obesity, overexertion, and spending a substantial amount of time on hard floors with your feet exposed and unsupported.
Fast and Easy
The therapy is actually a simple process that can leave patients feeling better the very next day. Shockwave therapy is not as dramatic as it sounds. It enables more blood flow to effected areas, addressing the source of the problem and allowing treatment to last for a long time.
Treatment & Recovery Time
Shockwave treatment will enable your feet to recover quickly. This is especially important since surgery is not required. It is cost effective and does not require the use of anesthesia. This treatment is a better option to surgery, since it is proven safe.
If you have any questions, please feel free to contact one of our offices located in Media, Glen Mills, Riddle Memorial Hospital, and Concordville, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Shockwave Therapy
Extracorporeal Shockwave Therapy (ESWT) is an alternative treatment method that is used for bone and soft tissue disorders in the foot and ankle. EWST is a noninvasive option for pain relief and it was originally created to help dissolve kidney stones. This therapy works by focusing impulses to target the area in pain. This method has been proven to show a reduction in the amount of nerve fibers that transmit painful impulses, which leads to a reduction in pain. Shockwave therapy can also expedite the tissue which would, in turn, increase the amount of new blood vessels that are formed.
Conditions that can be treated with shockwave therapy include Achilles pain and heel pain. People with plantar fasciitis may opt for this therapy and the results are usually great after 18 months. Additionally, this method can also be used to treat fractures that have failed to heal correctly. Anesthesia is not required to perform this treatment. It usually is not painful, but it can be uncomfortable.
The duration of treatment sessions usually lasts 5-15 minutes each. This procedure is safe since there is no risk of infection from wound complications, if you are looking to try shockwave therapy to heal plantar fasciitis, it may take 3-4 sessions to start working. After treatment, patients typically notice a dull pain in the area which was treated. However, this pain rarely lasts more than 24 hours.
Nevertheless, there are pros and cons that come along with Shockwave Therapy. The most obvious pro is that this treatment is noninvasive, meaning surgery will not be required. Another upside is that there have been very little complications that have been found with this procedure. On the other hand, those who opt for surgery are at risk for continued pain, wound problems, and infections. The biggest con for ESWT is that it is very expensive; it typically costs around $1,000 before insurance. Another con is that the effectiveness of the treatment is questionable. Usually, if this treatment is helpful, the difference is small.
If you are curious about Shockwave Therapy, you should talk to your podiatrist to see if this treatment method is right for you. At times, patients will find that there are other treatment options that are more efficient for their individual cases.
Understanding Hammertoes
 If you have hammertoes, it may be due to a number of factors including improperly-fitting shoes or muscle and nerve diseases that can affect your feet. Hammertoes are described as bent and curled toes, seeming to resemble the claw of a hammer. The condition is permanent and may require treatment if pain progresses. Typical treatment includes wearing the proper footwear and physical therapy. A final option is surgery for severe cases, but consulting with your podiatrist first about your condition is recommended before deciding on the surgical option.
If you have hammertoes, it may be due to a number of factors including improperly-fitting shoes or muscle and nerve diseases that can affect your feet. Hammertoes are described as bent and curled toes, seeming to resemble the claw of a hammer. The condition is permanent and may require treatment if pain progresses. Typical treatment includes wearing the proper footwear and physical therapy. A final option is surgery for severe cases, but consulting with your podiatrist first about your condition is recommended before deciding on the surgical option.
Hammertoe
Hammertoes can be a painful condition to live with. For more information, contact one of our podiatrists from Sutera and Jones Surgical Podiatry. Our doctors will answer any of your foot- and ankle-related questions.
Hammertoe is a foot deformity that affects the joints of the second, third, fourth, or fifth toes of your feet. It is a painful foot condition in which these toes curl and arch up, which can often lead to pain when wearing footwear.
Symptoms
- Pain in the affected toes
- Development of corns or calluses due to friction
- Inflammation
- Redness
- Contracture of the toes
Causes
Genetics – People who are genetically predisposed to hammertoe are often more susceptible
Arthritis – Because arthritis affects the joints in your toes, further deformities stemming from arthritis can occur
Trauma – Direct trauma to the toes could potentially lead to hammertoe
Ill-fitting shoes – Undue pressure on the front of the toes from ill-fitting shoes can potentially lead to the development of hammertoe
Treatment
Orthotics – Custom made inserts can be used to help relieve pressure placed on the toes and therefore relieve some of the pain associated with it
Medications – Oral medications such as anti-inflammatories or NSAIDs could be used to treat the pain and inflammation hammertoes causes. Injections of corticosteroids are also sometimes used
Surgery – In more severe cases where the hammertoes have become more rigid, foot surgery is a potential option
If you have any questions please contact one of our offices located in Media, Glen Mills, Riddle Memorial Hospital, and Concordville, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Blog Archives
- April 2025
- March 2025
- February 2025
- January 2025
- December 2024
- November 2024
- October 2024
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016
- May 2016
- April 2016
- March 2016
- February 2016
- January 2016
- December 2015
- November 2015
- October 2015
- September 2015
- August 2015
- July 2015
- June 2015
- May 2015
- April 2015
- March 2015
- February 2015
- January 2015
- December 2014
- November 2014
- October 2014
- September 2014